The New Medicaid
Stanley Feld M.D.,FACP, MACE
President Obama let the regulation to increase Medicaid reimbursements to the level of Medicare reimbursement expire because it failed to accomplish its goal. The goal was to get more physicians to accept Medicaid.
The Obama administration has proposed new federal regulations for Medicaid managed-care plans.
These regulations pledge the program's beneficiaries will have adequate access to a doctor. The pilot programs for these new regulations have been completed.
Two years ago six states made a deal with the Obama administration. Arkansas, Indiana, Iowa, Michigan, New Hampshire and Pennsylvania were willing to cover families earning up to 138% of the federal poverty level as long as it was on the states' terms.
Each state relies on private insurers, which are required to come up with qualified health plansthat meet the standards of Obamacare.
While Medicaid plan “purchasers” are almost totally subsidized, five of six states require some of these very low-income beneficiaries to make financial contributions that range as high as 2% of their income.
The idea is that everyone has some skin in the game. The plans also focus on setting up health savings accounts for beneficiaries and establishing wellness programs.
“While these are common features in many of today's corporate-sponsored plans (with only limited evidence to support claims that “more skin in the game” and wellness incentives hold down costs), these elements discourage enrollment by people who are scrambling to keep food on the table and a roof over their heads.”
I think the Obama administration is making another complicated mistake. There is not enough incentive in the program for Medicaid patients to try to save money for the government.
There is not enough incentive for physicians to sign up to accept Medicaid.
The Obama administration is using surveys of Medicaid beneficiaries.
“Their response is not much different from the perceptions of Medicare beneficiaries and the privately insured.”
“But closer examination, experts say, reveals that beneficiaries' satisfaction is boosted by the additional access that comes from visiting hospital emergency departments and government-subsidized community health centers.”
The Obama administration now proposes to hold Medicaid managed-care plans to the network adequacy of Medicare Advantage and Exchange Plans.
The six states, Arkansas, Indiana, Iowa, Michigan, New Hampshire and Pennsylvania, have been doing this along with offering higher-than-Medicaid rates to primary-care physicians to attract more of them to their networks.
A reduction in cost starts by managing patients in ways that encourage them to visit the doctor's office instead of the Emergency Department.
It does not have an element of encouraging patient responsibility or providing indigent patients with financial incentives to be financially responsible for their health or health care.
The same mistake is made over and over again. It is focused on providing patients healthcare coverage. The Medicaid Advantage healthcare coverage plans make Medicaid patients dependent on the government. It does not provide incentives for Medicaid patients to be responsible for themselves.
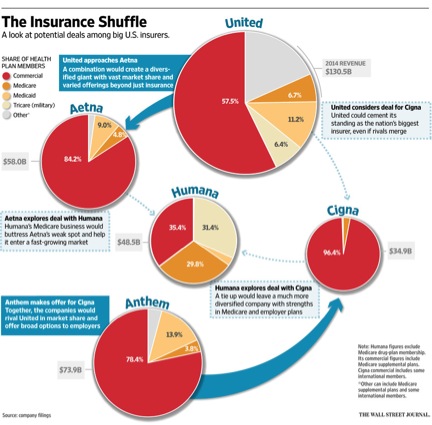
The healthcare insurance companies are planning to have a field day at the expense of the Obama administration. It seems like the Obama administration does not care how much the new plan costs.
The Obama administration is overlooking the important point. Healthcare coverage cannot work as long as patients are dependent on the government. Patients must be given financial incentives to be responsible for themselves.
All of the healthcare insurance companies that participate in the government supported medical insurance plans are aware of the impending changes in Medicaid.
These insurance companies bid for the administrative services contracts in each state.
The government makes the rules for engagement but the individual healthcare insurance companies bid for the contract.
It is totally logical for all the healthcare insurance companies attempted to merge. If these insurance companies were permitted to merge it would make Medicaid, Medicare and private insurance unaffordable to all.
The healthcare insurance industry sets the prices for administrative services.
The price increases would lead to citizen protest. It would lead to total government takeover of the healthcare system and a single party payer system.
http://money.cnn.com/2015/06/22/investing/health-insurers-mergers-cigna-anthem/
The CMS has released a sweeping proposed rule (PDF) intended to modernize the regulation of Medicaid managed-care plans.
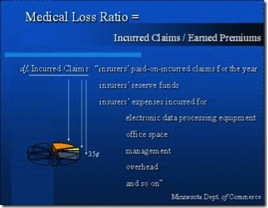
CMS plans call for health plans to dedicate a minimum portion of the rates they receive toward medical services, a threshold known as a medical loss ratio.
At the very last minute the Obama administration is proposing an 85% threshold for Medicaid managed-care plans, the same as the government’s regulations for large group plans in the private market.
The formula is MLR= incurred expenses /premiums earned.
Private insurance and Medicare are subject to an 85% MLR. It means that 85% of the premiums earned must go to direct medical care. Seventy five percent means only 75% must go to direct medical care and 25% can go to expenses as opposed to 15%.
The healthcare insurance industry also defines direct medial care expenses such as network formation, insurance salesmen’s commissions and other into the direct medical care column.
As of 2015, plans doing business with Medicaid and the Children's Health Insurance Program are the only health plans that aren't subject to an MLR.
The Medical/Loss ratio is one large source of profit to the healthcare insurance industry for two reasons.
Each expense allowed goes into the incurred claims column. The insurance industry builds a cost plus profit into each expense.
- The more required services (Obamacare requirements) rendered by that insurance company the more fee for those services which include profit goes into the incurred claims column.
- Each expense allowed goes into the incurred claims column. The insurance industry builds a cost plus profit into each expense.
- The more premiums collected the more goes into expenses in the incurred claims column.
- The lower the percentage (85% to 75%) of the Medical/ Loss Ratio profit to the healthcare insurance company.
“An arbitrary cap on health plans' administrative costs could undermine many of the critical services—beyond medical care—that make a difference in improving health outcomes for beneficiaries, such as transportation to and from appointments, social services, and more,” interim AHIP CEO Dan Durham said in a statement."
The MLR that the CMS has proposed for Medicaid plans is a suggestion rather than an enforceable mandate.
Medicaid managed-care enrollment has soared by 48% to 46 million beneficiaries over the past four years, according to consulting firm Avalere Health. By the end of this year, Avalere estimates that 73% of Medicaid beneficiaries will receive services through managed-care plans.
"This proposal will better align regulations and best practices to other health insurance programs, including the private market and Medicare Advantage plans, to strengthen federal and state efforts at providing quality, coordinated care to millions of Americans with Medicaid or CHIP insurance coverage.”
America's Health Insurance Plans immediately said applying an MLR to Medicaid managed care fails to reflect much of what these managed care plans do to hold down costs.
In essence the new Medicaid proposal will also fail if the healthcare insurance industry merges and the impending fight over the MLR continues.
The cost of healthcare insurance will increase for the private sector, Medicare and Medicaid.
The fault lies in President Obama's lack of understanding in who should drive the healthcare system. Consumers should drive the healthcare system not the government.
The opinions expressed in the blog “Repairing The Healthcare System” are, mine and mine alone
Please have a friend subscribe