Actions Contradicts Goals
Stanley Feld M.D.,FACP,MACE
The
promise of Obamacare is to deliver quality medical care at an affordable price.
Prevention has been emphasized. Prevention will avoid costly complications of a
disease.
The talk about prevention is excellent. The healthcare
policy action falls short of the promise.
Despite strong efforts by the International Society
for Clinical Densitometry and other sister societies in the Fracture Prevention
Coalition, a provision to increase Medicare payments for DXA was not included
in the fiscal cliff legislation.
Congress adopted the American Taxpayer Relief
Act of 2012, HR 8, on January 1, 2013. The bill included a number of other
provisions affecting Medicare payments to physicians that have caused disappointment. The
bill did not include the need to incentivize the use of bone density for the
early diagnosis of osteoporosis.
Below is
a summary of how the various Medicare provisions were resolved in the act and
the bottom line for DXA:
1. The new law blocks the 27% Medicare physician payment cut resulting
from the Sustainable Growth Rate (SGR) formula, freezing
Medicare payments at the 2012 level through calendar year 2013.
2. The automatic "sequestration" cuts that would also
have reduced Medicare physician payments by another 2% are postponed
for two months until 3/1/12013.
3. The bill authorizes cuts to reimbursement for advanced
imagining services such as MRI and CT. These cuts do NOT apply
to DXA, which is not considered an advanced imaging service.
As a practical matter, the new payment rate for DXA in the office setting
dropped on 1/1/2013 from a national average of $56 to $50.
I have written about the definition of quality medical care for osteoporosis.
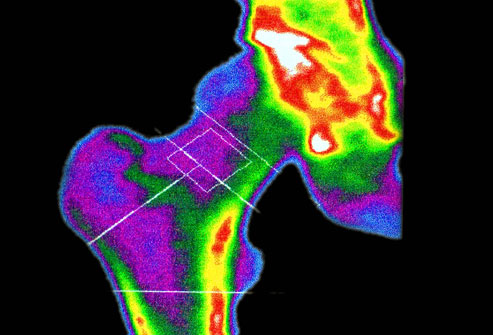
Osteoporosis can be diagnosed early by bone densitometry (DXA). Osteoporosis
is a progressive disease.
Discouraging the use of DXA is not a step in the right direction for preventing
costly complications.
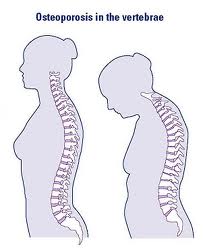
Osteoporosis affects the spine (vertebral column). It is initially manifested
by a decrease in bone density as determined by DXA. As osteoporosis progresses
patients develop compression fractures. Some compression fractures are painful
and some are not.
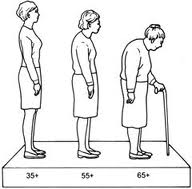
Patients lose height and develop a stooped posture.
The change in patients’ posture causes a change in the patients’ center
of gravity. The change in the center of gravity causes a change patients’
ability to balance herself against a fall.
If patients with osteoporosis fall they can put torsion on their hips.
The bone in the hip is thinned by the long process of developing osteoporosis.
Their hips can fracture.
The mortality rate after a hip fracture is more than 20%. The morbidity rate
post- op is 40-50%. Very few patients return to having a normal quality of
life.
Patients may be forced to live in nursing homes.
If we look at elderly people around us we will notice that as many as 60%
of people over 70 years old have lost height and are have stooped posture. They
have osteoporosis.
Early osteoporosis starts manifesting itself at about 50 years in women
and 70 years old in men.
Modern medicine can prevent the onset of osteoporotic fractures. Modern
medicine can also prevent further fracture by treating women and men after they
have developed osteoporotic fractures.
Preventing hip fractures would save the healthcare system billions of
dollars a year in healthcare expenditures. Prevention of further fractures
would also increase the quality of life in elderly osteoporotic patients.
Much has been written about the IPAB (Independent Physician Advisory
Board). I have written about the
potential defects in the structure of this board and the defects and
functioning of its existing precursor the USPSTF (United States Preventative Services
Task Force).
The USPSTF recommendations are created from its review of the published
literature. Most of the committee members are non-specialists. They do not have medical experience in
treating osteoporosis. The committee ignores the consideration of the natural
history of the disease.
Yet, the USPSTF recommendations have resulted in a yearly decrease in the
reimbursement by both private insurers and Medicare for bone densitometry (DXA).
In some cases private insurers and Medicare do not pay. This is the way
to restrict access to care and devalue physician' judgment.
Physicians have not done a good
job detecting and treating osteoporosis. The decrease in DXA reimbursement will
further decrease physicians’ interest in treating osteoporosis preventively.
A small short-term cost savings will result in increased long-term expenditures.
The result will be an increase in cost to the healthcare system.
This is the contradiction in Obamacare’s promise of prevention.
Prevention is the key to healthcare savings.
The opinions expressed in the blog “Repairing The Healthcare System” are, mine and mine alone.



nursing homes in birmingham • February 3, 2013
nursing homes in birmingham
Repairing the Healthcare System: Actions Contradicts Goals
Polymoist cream • February 9, 2013
Polymoist cream
Repairing the Healthcare System: Actions Contradicts Goals