Healthcare Insurance Industry’s’ New Business Model Is Wrong.
Stanley Feld M.D.,FACP,MACE
One percent of the people spend 25% of the healthcare dollars. Twenty percent of the people spend 80% of the healthcare dollars.
It would be important to know why this is true. Then figure out what could be done about it Stakeholders need to agree on a course of action.
It would be a good idea to understand what physicians think should be done.
“One percent of patients account for more than 25 percent of health care spending among the privately insured, according to a new study. Their medical bills average nearly $100,000 a year for multiple hospital stays, doctors’ visits, trips to emergency rooms and prescription drugs.”
The 1% and the 20% are suffering from complications of a chronic disease.
The incidence of chronic diseases is on the rise in the United States. A major precipitating factor for this is obesity.
The incidence of Type 2 Diabetes Mellitus is increasing in both adults and young children, as the incidence of obesity is increasing.
The incidence of complications of Diabetes Mellitus will increase in the future. The result will be an increase in the cost of medical care.
President Obama’s healthcare reform act will expand healthcare coverage to 32 million uninsured in 2014. Obamacare is forcing the healthcare insurance industry to change its business model in order in order to remain profitable.
Premiums are out of the reach of most businesses and individuals. Premium increases are not an option.
High-risk individuals are denied healthcare insurance coverage. High-risk patients automatically get coverage in corporate healthcare plans. The healthcare insurance industry simply raises premiums on corporate groups in order to maintain its profits.
Something must be done to decrease the increase in chronic disease and its complications.
The government cannot afford to insure its present patient obligations much less the 32 million uninsured.
“As the new federal health care law aims to expand care and control costs, the people in the medical 1 percent are getting more attention from the nation’s health insurers.”
Twenty percent of the population not 1% should be getting the attention of the healthcare insurance industry.
“Studies have already shown that Medicare spending is concentrated on a small group of individuals who are seriously ill.
An analysis by the IMS Institute for Healthcare Informatics, the research arm of IMS Health, a health information company in Danbury, Conn., provides a rare glimpse into the medical problems of people with private health insurance that are under 65.
About three-quarters of them suffer from at least one chronic condition that could spiral out of control without proper care.”
Most of these people were obese.
The healthcare insurance industry cannot avoid these patients after 2014.
“Insurance companies will be required to enroll millions of new customers without the ability to turn them away or charge them higher premiums if they are sick. They will prosper only if they are able to coordinate care and prevent patients from reaching that top 1 percent.”
The healthcare insurance industry realizes it must fundamentally change its business model.
The healthcare insurance industry has a problem developing a new business model that would work. The industry does not want to lose control over patients, their physicians and the monies paid into the healthcare system.
The healthcare industry does not have a clue about how to actually repair the healthcare system. It is focused on its own bottom line rather than looking at business models that will be beneficial to everyone and align all the stakeholders’ incentives.
The healthcare insurance industry is planning on instituting programs that will tinker with the edges. It will not fix the problems.
The new business models will increase the percentage of money the insurance industry receives for direct patient care maintaining a Medical-Loss ratio of 15%. There is no interest in providing patients with financial incentives and a choice.
The net result will be higher costs and system failure. The weird thing is most of the healthcare insurance industry executives know it.
“The reality is if we don’t figure out how to get to the patients, we’re not going to get where they need to be,” said Dr. Lonny Reisman, the chief medical officer for Aetna.
The reality is that the system must be consumer driven with consumers in charge of their healthcare and their healthcare dollars.
At the moment patients have no incentive to decrease the cost of care. Hundreds of patients have told me that they go to the doctor to fix their illness. Medicare or their insurance pays. The patients have no idea of the costs they incur nor do they care. They have no interest in controlling their disease.
My ideal medical saving accounts would give the patients incentive to learn about their disease. They would be interested in self-managing their disease with the physician and his medical care team being the coach.
“The next challenge, say insurers, is to figure out how best to work with a person’s doctor. Because many of these patients seem to be seeing many doctors and taking many medications, there may be no one who is accountable for the patients’ overall health.”
Physicians have figured out what services get paid by the healthcare insurance industry. They do not get paid for educating patients about their disease.
The healthcare insurance industry and the government have developed a punitive bureaucracy.
An attempt is being made to penalize or reward physicians for medical outcomes. Pay for Performance (P4P) is a punitive payment system. It will fail.
Patients are responsible in large part for the onset of their medical problems and in controlling their medical outcomes. Physicians cannot be responsible for patients’ outcomes. It is the responsibility of the patient.
“Insurers are also still grappling with their understanding of human nature — why some people simply don’t take care of themselves or take their medicine or go to the doctor, even when it is clear that they should.”
Patient outcomes have nothing to do with human nature. It has everything to do with financial incentive and effective education.
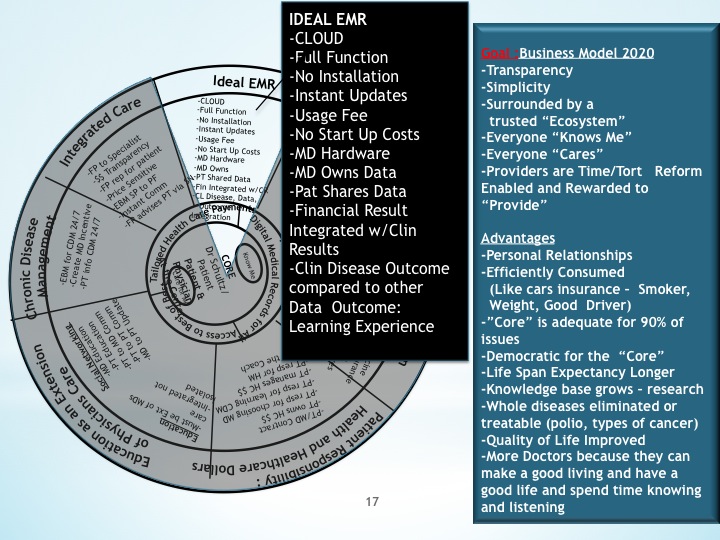
Spokes 5 and 6 of my future state business model has everything to do with patients’ responsibility for caring for their disease and the physicians’ responsibility to the patients. It has nothing to do with physicians’ and patients’ responsibility to the healthcare insurance industry or government.
The opinions expressed in the blog “Repairing The Healthcare System” is, mine and mine alone
Please send the blog to a friend