Chronic Disease Management And Education As An Extension of Physicians’ Care.
Stanley Feld M.D.,FACP,MACE
All the Spokes in my Future State healthcare business model should be attended to simultaneously to be effective.
My vision ignores the barriers of the journey to implementing the changes in this discussion. There will be many barriers. Legacy vested interests find it difficult to see a better way when those interests are struggling to survive in the present system.
The healthcare system must be consumer driven. Consumers must be put in control of their healthcare dollars. The other stakeholders will then be forced to cater to the consumer.
When this happens all the stakeholders’ vested interests will become aligned. It will result in a decrease in healthcare costs and an increase in stakeholders’ satisfaction.
Patients will accept responsibility for the management of their health. Physicians will become more efficient in their delivery of care..
The music industry fought Apple after ITunes dis-intermediated its legacy business model only to find its profit increased.
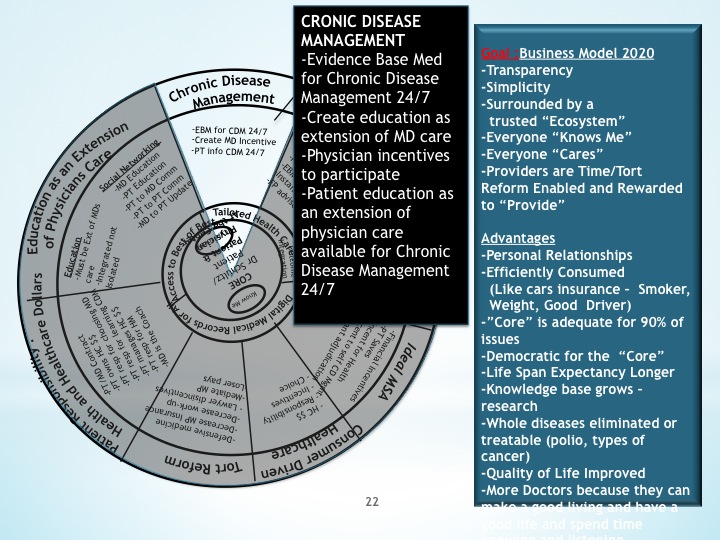
Consumers must have a way to obtain adequate chronic disease management education. They must have transparent healthcare costs and understand treatment choices. Physicians must be actively involved in their patients’ education.
Chronic disease management education must be an extension of the physicians’ care. It is part of patients’ medical care. Physicians must be motivated to provide this care.
Effective chronic disease management is dependent on patients managing their chronic disease. Patients will take control only after appropriate incentives and educational methods are in place.
The goal is to decrease the onset of complications of a chronic disease. Patients can control their disease and decrease the occurrence of chronic complications. Eighty percent of the cost of medical care is spent on treating these complications.
Physicians must teach patients to become the professor of their chronic disease. The educational vehicle must be available 24/7 for patients to be able to review concepts they did not understand completely.
Physicians must have knowledge of current evidence based medical care to teach patients properly.
Much of the infrastructure is in place. It tends to be provided by secondary stakeholder and undermines the patient physician relationship. The infrastructure is not utilized properly.
Patients need to be responsible for controlling their disease. Chronic disease management is not an entitlement. It is a patient responsibility.
Patients are dependent of the government or the healthcare insurance industry to pay their bills. They have first dollar healthcare coverage
My ideal medical saving account would solve this issue. It would probably cost the government and the healthcare insurance industry less if they provided patients with $7,500 in a trust fund, provided the incentives for keeping money not spent and provided first dollar coverage after the patient spends $7,500 dollars.
Patients will then be converted to Prosumers (Productive consumers) and become intelligent consumers of healthcare.
Consumers would then encourage or force their physicians to provide appropriate chronic disease management education.
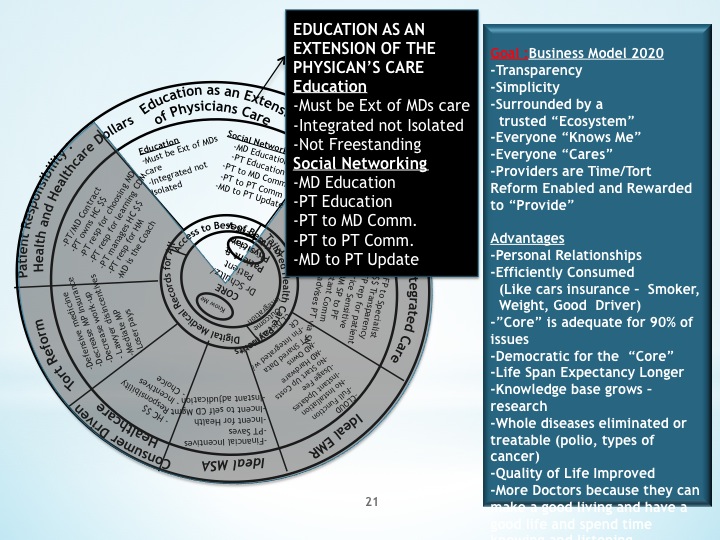
The formation of social networking on multiple levels could enable physicians to provide this education inexpensively and effectively.
For example, all of a physician’s diabetics patients can be members of his social network for diabetics. The information to learn about diabetes can be provided by his social network. Testing of patients’ understanding of core principles of diabetes can be done with direct feedback to the physician. This would provide the physician with insight to emphasize topics the patient did not understand.
The core information could also default to a more detailed explanation of the topics misunderstood.
It could be done for many chronic diseases such as asthma, COPD, heart disease, GI diseases, and joint diseases.
This education would promote the physician patient relationship. It would demonstrate than their physicians care about their care.
If there is a contradiction in the education between the physician’s thinking and the core information, a separate social network connected to the core information for physicians only can serve as a platform for debate between physicians. Continuing medical education could even be provided to give physician incentive to participate.
There are many innovative mechanisms to use to promote the patient-physician relationship, educate patients to be professors of their disease, and to be responsible for their own disease management.
The utilization of information technology through social networking will repair the healthcare system. It will enable access to education and affordable care.
The opinions expressed in the blog “Repairing The Healthcare System” is, mine and mine alone
Please send the blog to a friend