President Obama Tries To Shut Up Media
Stanley Feld M.D.,FACP,MACE
On April 16th President Obama tried to shut up the media’s criticism of Obamacare with his announcement that 8 million people have enrolled in Obamacare. The administrations had reached its goal. Obamacare is a success
Mr. Obama pointed to the number to declare the law a success and that Republicans should stop trying to overturn it.
"The point is, the repeal debate is and should be over," the president said. "The Affordable Care Act is working and I know the American people don't want us spending the next 2½ years refighting the settled political battles of the last five years."
One month earlier we heard from the same administration that the 6.6 million people who had lost their healthcare insurance because of Obamacare was an insignificant sliver of the population.
President Obama’s announcement contained few new details about enrollment.
The entire point of Obamacare was supposed to be to insure people who were uninsured previously.
It turns out (from insurance company data) that as many as 80% of the 8 million enrollees were replacing extremely expensive healthcare insurance policies with Obamacare healthcare policies.
Individual healthcare insurance for older people with a pre-existing disease is unobtainable or extremely expensive.
These people were in the individual healthcare market only. Many had pre-existing diseases and chronic diseases.
Their risk is much higher than low risk patients. Many of these people received government subsidies because they made less than $50,000 dollars a year.
The administration has still not published the number of people who did not have insurance before Obamacare went into effect and have signed up and paid their premium.
President Obama claims he does not know that number. If the healthcare insurance companies know the exact number the Obama administration has to know that number.
President Obama’s declaration of success is ludicrous.
Patients who enrolled and paid their premium are going to realize the negative impact it will have on their medical care shortly.
There is no class of American professionals who will be more negatively impacted by Obamacare than physicians.
Obamacare reinforces the worst features of third-party payment arrangements for payment of medical care. The third party payment system of healthcare insurance has already compromised the independence and integrity of the medical profession.
“With Obamacare physicians will be subject to more government regulation and oversight, and will be increasingly dependent on unreliable government reimbursement for medical services. “
These are some of the difficulties physicians will face with Obamacare.
The Medicare Payment Formula is flawed. Physicians continue to face the threat of deep payment cuts under Medicare’s sustainable growth rate (SGR) formula.
The SGR governs the annual growth of Medicare physician payments. Congress has kicked the can down the road since 2003. Physicians have incurred a potential reduction of 30% from the present payments if congress does not provide a permanent fix.
Medicaid will be expanded in states that agree to do so to cover any individual earning up to 138 percent of the federal poverty level—$15,856 for an individual in 2013. Many states have refused to expand Medicaid.
The Congressional Budget Office (CBO) projects that this expansion will add 12 million individuals to Medicaid by 2015.
The physician reimbursement rates for Medicaid patients is 58% lower than the reimbursement physicians receive in the private sector.
Thirty three percent of physicians do not participate in Medicaid. Patients’ access to physicians is decreased. The result is Emergency room overcrowding. ER overcrowding was the very thing the President Obama’s healthcare policy wizards wanted to decrease.
Obamacare is imposing more bureaucracy, rules, regulations, and restrictions on physicians.
Since 2010, with few exceptions, the law prohibited physicians from referring Medicare patients to hospitals in which they have ownership.
- Thus, a whole class of physician-owned, specialty hospitals has been removed from competition, even though they enjoyed an undisputed record of providing high-quality patient care.
- This regulation has driven a large number of physicians to stop accepting Medicare even thought their service is of high quality and less expensive than hospital systems.
- There have been mountains of new regulations that are impossible to keep up with. These regulations have driven physicians away from accepting Medicare reimbursement.
- Obamacare has created multiple federal agencies, boards and commissions to regulate the practice of medicine.
- These creations are partly the fault of physician groups not effectively regulating their peers.
a. Obamacare created a “nonprofit” Patient-Centered Outcomes Research Institute. The institute will determine clinical effectiveness of medical treatments, procedures, drugs, and medical devices.
The result will be an administrative implementation nightmare. All medicine is local. Only financial incentive can work. Penalties and regulatory requirements will not work. It will simply generate an atmosphere of mistrust and non-cooperation.
The Patient-Centered Outcomes Research Institute could be a teaching tool for physicians and patients.
However, the likelihood of the government dictating cookbook care guidelines and regulations, and interfering with physicians’ clinical judgment and the further destruction of the patient-physician relationship is high. The Institute will also retard clinical innovation in the delivery of care.
The goal is to reduce the growth rate of Medicare spending and non-federal spending through health insurance exchanges.
The chance of congress presenting an alternative equivalent saving is small. President Obama has stated in the past that the IPAB has little power except to make recommendations. This is not true!
Former Vermont Democratic Governor Howard Dean (D) has said,
"IPABs are essentially a health-care rationing body. By setting doctor reimbursement rates for Medicare and determining which procedures and drugs will be covered and at what price, the IPAB will be able to stop certain treatments its members do not favor by simply setting rates to levels where no doctor or hospital will perform them."
This is the only thing that Dr. Dean has ever said that I have ever been able to agree with.
The IPAB will control spending through reimbursement cuts. It can enable limited or no payment for selected services and medical procedures or for Medicare physician payment.
It looks as if it could drive physicians out of practice and hospital out of business. This is especially true in the absence of tort reform.
c. Pay-for-performance programs are another terrible idea. Physicians can only control some of the outcomes. Patients’ compliance/adherence is the key to most outcomes.
Payment will be adjusted to reflect performance. The measurement will be based on data from the Physician Quality Reporting System and cost data from Medicare fee-for-service claims.
I have previously demonstrated the ineffectiveness of using claims data to make outcomes decisions.
These programs can be used to create powerful economic incentive by complying with standardized guidelines at the expense of individual patient care.
All you have to do is “check the box” to achieve a high and financially beneficial score as a condition of participating in the government’s health programs.
It is aa attempt created by bureaucrats that will not work in the real world.
Most physicians hate Obamacare. Forty-three percent of physicians are considering retiring in the face of the need for an additional 91,500 physicians by 2020.
“Obamacare neglects physicians’ most pressing concerns, such as tort reform, and significantly worsens the already painful problems that come with third-party payment and government red tape.”
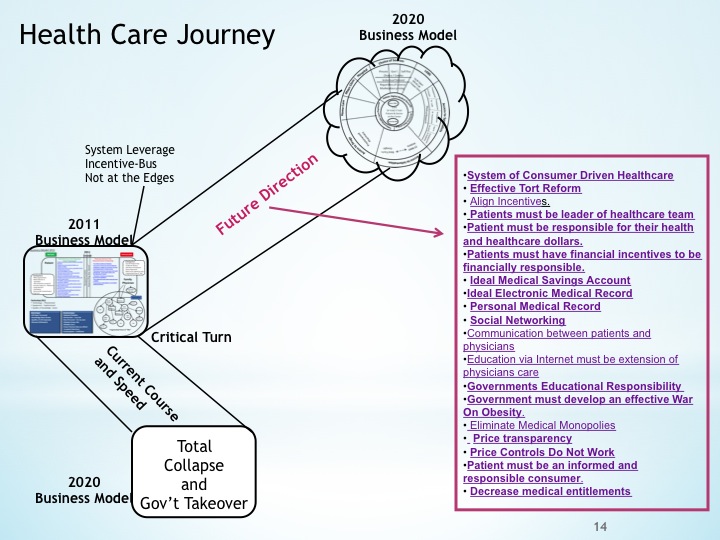
Obamacare misses all the keys necessary for Repairing the Healthcare System. Obamacare steers out of the skid (wrong direction). It makes things worse.
Consumers must drive the healthcare system. The physician/patient relationship must be restored. Physicians must help patients make treatment decisions not government, insurance executives and other bureaucrats.
Repairing the Healthcare System will not be achieved until patients, not the government, control their health care dollars and decisions at the advice of their physicians in a viable physician patient relationship.
My Ideal Medial Savings accounts steer into the skid and repairs the healthcare system.
The Obamacare debate is hardly over as President Obama has declared.
The opinions expressed in the blog “Repairing The Healthcare System” are, mine and mine alone
Please have a friend subscribe