Obamacare Drives Premiums Up In 45 Of 50 States
Stanley Feld M.D.,FACP, MACE
President Obama promised
during his campaign for passage of the Affordable Care Act that the Act would
cause premiums "for the typical family" to fall by $2500.
He also said it would bend
the healthcare cost curve and if you like your doctor you can keep him or her.
We all remember these sound bites. The sound bites are all turning out to be
false.
Many intelligent people who
believe in Obamacare refuse to consider these facts. I can understand the
denial.
They will pay attention as
soon as it effects them.
The added required benefits mandated
in insurance coverage in the law and the way the healthcare insurance industry
is permitted to calculate its Medical Loss Ratio makes President Obama’s
calculation impossible.
President Obama has been telling
the American public a lie all the while. People are starting to understand.
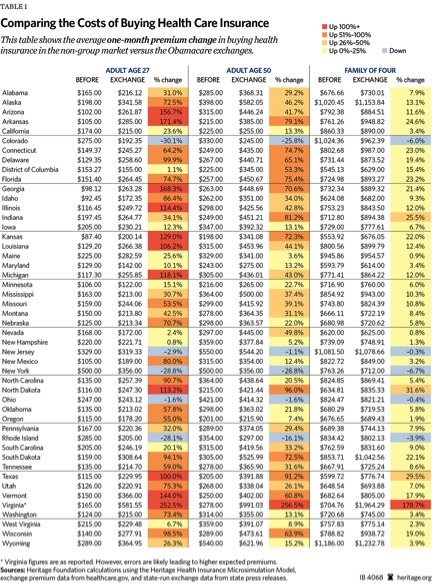
The average one month premium
change from buying insurance in the non-group market in 2013 versus the
Obamacare exchanges in 2014 is not revealed in any government statistics. Two
studies were completed by private sources.
Premium comparisons between
2013 and 2014 are not available from Health and Human Services (HHS).
The 2013 premiums increased
by double digits from the 2012 premiums because of Obamacare. The traditional
media has not pressed the government to provide these comparisons.
The media continues to quote
the administration press releases of lower premium prices. The Obama administration uses CBO estimates
of premium prices calculated in 2010 for 2016 by data provided by the Obama
administration. The tradition media refuses to report reality.
Premiums paid outside the
health insurance exchange will increase the same percentage or more.
No one can
say the American public has not been warned.
There is
going to be tremendous public outcry in the individual market for insurance
when the cost to individuals and the American taxpayers is realized.
October
1,2013 is open enrollment season for the individual and group insurance market.
President
Obama has exempted the group market from Obamacare until 2015.
One of the
reasons for the exemption for the group market is to try to mute the outcry by
splitting the non group insurance from the group insurance holders.
Some of the
premium increases have already been report in the traditional media.
The Department of Health and Human Services published a similar
report. The government’s report is incomprehensible to me.
It does not compare pre Obamacare premiums of 2013 to
Obamacare Health Insurance Exchange premiums of 2014.
—Douglas
Holtz-Eakin
President, American Action Forum[1]
The Department of Health and Human Services has
declared a 16% decrease in premium costs compared to the CBO’s 2010 estimate of
premiums for 2016.
It is important to remember the CBO’s
calculation was with faulty data provided by the administration.
“Based on a Manhattan Institute analysis of the HHS numbers,
Obamacare will increase underlying insurance rates for younger men by an
average of 97 to 99 percent, and for younger women by an average of 55 to 62
percent. Worst off is North Carolina, which will see individual-market rates
triple for women, and quadruple for
men.”
The Obama
administration’s methods of deception are cunning, powerful and effective.
He always blames others and hides his ideology.
President
Obama continues to try to fool a majority of the people most of the time.
Americans will
get the point where the rubber meets the road. The public is going to
have to reach into their pockets and pay these enormous increases in premiums
or not buy healthcare insurance coverage.
Taxpaying
Americans are also going to experience massive increases in taxes above and beyond those already experienced.
I predict the
public outcry will drown out the spin of the Obama administration. The
traditional media will not be able to ignore this public outcry.
People will
finally realize the enormous government grab of power and control of Obamacare at
taxpayers’ expense.
People
can’t complete applications or secure premium prices on the health insurance
exchanges because of technical problems resulting from ancient information technology
used by the government to construct the exchanges.
All of the
consumers’ demographics must be filled out before the government provides a
premium price. There is at tricky reason for this.
This
computer “glitch” solidifies my view that President Obama wants Obamacare to
fail in order to replace it with a single party payer system that America
cannot afford.
This last
statement is counterintuitive but I believe true.
Is it wise
for consumers to hand over all their medical decision making to a government
that has this much difficulty with executing a computer program and providing
healthcare insurance premiums?
Americans
must wake up soon. They have to insist on a consumer driven healthcare system
in which they have control over their healthcare and their healthcare dollars.
Americans have
to insist on having an Ideal Medical Saving Account healthcare system.
I have described the Ideal Medical Saving Account System in great detail.
The opinions expressed in the blog “Repairing The Healthcare System” are, mine and mine alone
Please have a friend subscribe