The Future State Business Model For Repairing the Healthcare System
Stanley Feld M.D.,FACP,MACE
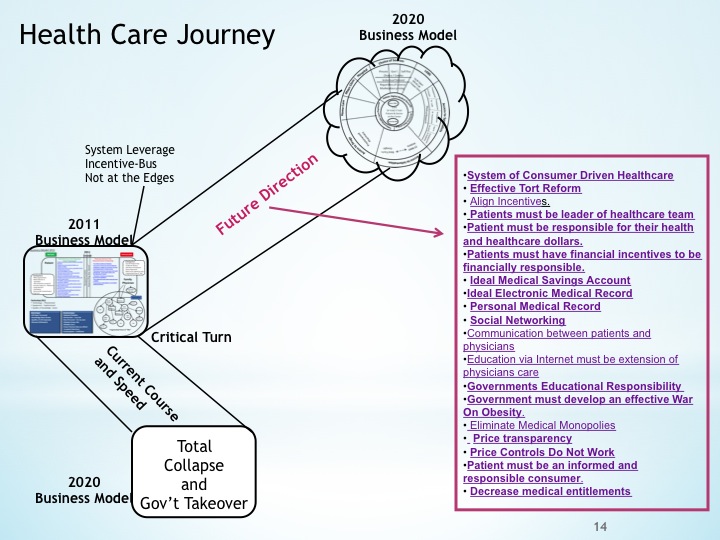
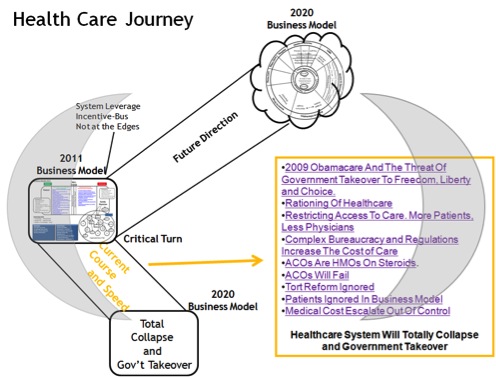
Obamacare is going to lead to the demise of both the healthcare system and the medical care system in the United States. America is at a critical turn in 2012. The evidence for the collapse is presented in the following links.
The business model for a successful repair of both the healthcre system and the medical care system are outline on the next slide.
A consumer driven healthcare system is critcal to a successful repair of the healthcare system. Read this link to understand the full meaning and implications of a consumer driven healthcare system.
Consumers must drive the systems by being responsible for their own healthcare decisions and own their healthcare dollars even if they are subsidized by the government.
Another critcal element in business model for the future state is effective tort reform. Ideally defensive medical testing has to be eliminated completely. Defensive medical costs the healthcare system between $300-500 billion dollars a year
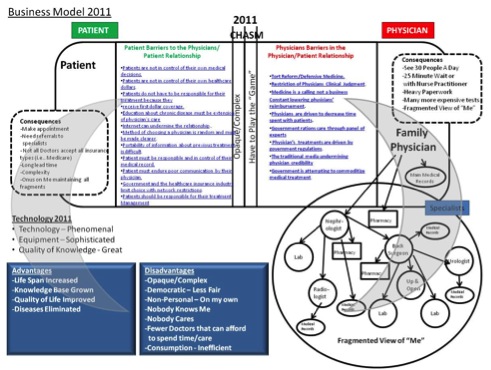
A summary of the misalign insentives must be understood and examine . There is a way to align all the primary and secondary stakeholders incentives. It must be agreed too that consumers are the primary stakeholders and physicians are next. Most of the control and power in the system has shifted to the secondary stakeholder namely the government, the hospital systems and mostly the healthcare insurance industry.
The government must understand that the only way to reduce cost is to shift the responsibility of controlling costs from the government to consumers.
Consumer must be the leader of their healthcare team.
Consumers must be responsible for health and healthcare dollars.
Consumers must have effective financial incentives to become medically responsible to themselves. It is clear with the incidence of obesity, the increases in smoking and drug addictions, hearth attacks, and strokes from high blood pressure that the need to attain good health is not enough incentive.
My ideal Medical Saving Accounts are an excellent way of providing financial incentives to achieve good health in a consumer driven system. The achievement of good health will drive down the costs to the healthcare system. The incidence of costly complications of disease will be reduced.
My ideal Electronic Medical Record is an important innovation. It is inexpensive to physicians. The data belongs to patients and their physicians and set up in a way that it is not punitive to physicians. It should be a fully functional EMR.
All physicians know that medical care decisions making and judging the quality of medical care by electronic data is faulty. All the EMR's are expensive. They also put physicians in a vulnerable position to be judged by faulty data. My Ideal EMR helps physicians track their patients and improve their medical communications and care.
It is important that consumer become responsible for their own Personal Medical Record. The ideal EMR permits patients to download their records with their tests to their own computer or flash drive. Consumers should carry their medical records at all times in case of emergency.
Social Networking is the key to a consumer driven healthcare system. The possibilities are compelling.
Improved communication between patients and physicians will be driven by a consumer driven healthcare system connected to social networking. The motivations is financial when consumers own their healthcare dollars.
Education via the Internet must be an extension of physician care.
Government's Educational Responsibility:
Teach consumers to become intelligent healthcare consumers
Government must develop a program to effectively combat obesity. There must be a change in the food industry and farm policy.
Patient must learn to be and educated and responsible healthcare consumer.
There must be a decrease in medical entitlement programs. Consumers must have skin in the game in order to be educated and responsible consumers. Consumers need to be a financial risk.
This is the outline of the future state business model. The readers should click on each link to read the details of each bullet point.
This business model will enable America to have an affordable healthcare system for all which will become sustainable.
The opinions expressed in the blog “Repairing The Healthcare System” are, mine and mine alone
Please have a friend subscribe