Stanley Feld M.D.,FACP,MACE
President Obama and progressive Democrats such as John Kerry and Barney Frank wanted the healthcare system to become a single party payer system. Their problem was that they could not get enough votes in the house or senate.
This goal for a single party payer by the progressives and Democrats must not be forgotten as the Trump administration tries to make a serious attempt to repair the healthcare system.
The Democrats and progressive will try to block this attempt at every turn.
All the stakeholders have played an important role in distorting the healthcare system including the government, the healthcare insurance industry, the pharmaceutical industry, the hospital systems, the physicians and patients.
A starting salary for a starting hospital administrator is $250,000 a year. A starting salary for a pediatrician is $90,000 a year. Top hospital administrators are paid between five (5) million and fifteen (15) million dollars a year. Mature pediatricians make $150,000 to $200,000 a year.
Which professional adds more value to medical care? Physicians add more value to the medical care system. Hospital administrators do not understand why physicians resent them.
Physicians also resent hospital systems ripping off consumers with $50 aspirins and $100 sleeping pillows. Consumers who care about the cost of healthcare do not understand why the government and insurance companies let hospital systems charge these obscene prices.
Most physicians do not pay attention to these costs until they are patients.
All of the stakeholders except the government and patients try to optimize the amount of money they take out of the system. Surgeons are much further ahead of primary care physicians in figuring out their value to the healthcare system.
As a result of advances in technology, physicians figured out that 70-80% of the work-ups done requiring hospitalization 30 years ago could be done as outpatient care.
The brick and mortar value of hospital facilities has decreased.
As soon as hospitals realized this they started to build ambulatory surgical care facilities and outpatient clinics. Hospital system procedures are more expensive than free standing outpatient ambulatory surgical care facilities.
http://stanfeld.com/hospital-mergers-dont-work/
Hospital administrators somehow convinced the government that if they formed hospital systems and merged hospitals in an area they would increase their efficiency and they could decrease costs.
At the same time the management of private practices became complicated as a result of government regulations. Expensive electronic medical records were required but did not work as advertised. Overhead increased while reimbursement decreased.
Many physicians became disgusted managing their complicated private practices. Some physicians quit practicing early.
The hospital systems offered to buy private practices for a “reasonable cash price”, provide an electronic medical record, do the billing and management of the practice and hire and pay full time employees.
Hospital systems usually paid physicians under contract the same take home pay they had for two years. After the two-year contract expired the hospital systems offered new contracts depending on a physician’s productivity or fired the physician. Physicians had no say in the matter.
Physicians and surgeons signing with the hospital system did not consider the criteria to be used for determining salary after their contract expired .
This hospital arrangement seemed attractive to many primary care physicians and some surgeons. The growth of hospital owned physicians increased from 20% to 70% of physicians in a region.
Organized medicine, the AMA and physician specialty groups, did little to warn or educate physicians of these unforeseen consequences.
Hospital systems did their best to isolate private practicing physicians from using their hospital facilities.
The only private practice physicians who were not marginalized by the hospital systems were physicians who were needed by the hospital system for the services they performed. As soon as the hospital systems were able to hire physicians to cover those services the private practice physicians were marginalized.
Large hospitals systems are making deals with insurers that squelch competitive hospitals.
President Obama’s plan was to allow hospital systems to hide prices from consumers and corporations. The goal was to discourage use of less-expensive rivals. This tactic would force the less-expensive competition to join the regional hospital systems as affiliates.
At first hospital systems did not grasp the ultimate significance of enlarging hospital systems. They figured merging hospitals would increase efficiency and decrease the cost of medical care.
They also thought owning physician practices would decrease their reliance on in-patient hospital billings and their brick and mortar structures.
During the Obama years there was a tremendous increase in building growth on the campus of most hospital systems.
I never understood the hospital building growth. More building meant more hospital administrators and more overhead. I thought the government must have created some economic incentive for hospital systems to build more buildings on campus. I could not find the incentives given to hospital systems.
As hospital systems merged all the hospitals in a region the hospital systems realized they had a monopoly on not only hospital services but also physician services.
They could negotiate with healthcare insurance companies from strength.
Initially the healthcare insurance companies were in control of the costs and services that were available. The healthcare insurance companies lost their control over cost to the regional hospital systems.
“Dominant hospital systems use an array of secret contract terms to protect their turf and block efforts to curb health-care costs. As part of these deals, hospitals can demand insurers include them in every plan and discourage use of less-expensive rivals. Other terms allow hospitals to mask prices from consumers, limit audits of claims, add extra fees and block efforts to exclude health-care providers based on quality or cost.”
There are hundreds of regional hospital system giants throughout the United States. In many cities there are two or three giant hospital systems. It is difficult for independents to negotiate contracts in these cities.
“The Wall Street Journal has identified dozens of contracts with terms that limit how insurers design plans, involving operators such as NewYork-Presbyterian, Johns Hopkins Medicine in Maryland, the 10-hospital OhioHealth system and Aurora Health Care, a major system in the Milwaukee market. National hospital operator HCA Healthcare Inc. also has restrictions in insurer contracts in certain markets.”
This is a very big deal.
The goal of the government should be to lower the price of healthcare to all of its citizens including seniors, workers who get insurance from their employers and people who do not have employer sponsored healthcare.
The Obama administration did nothing about stopping hospital system monopolies. In fact, it encouraged them.
“Certain hospital systems are able to command advantageous terms because they have grown through years of deal-making, shifting the balance of power between hospitals and insurers. In 2010, the year the Affordable Care Act passed, the annual number of hospital mergers shot up 40% to 59, and the number of deals has remained above 60 every year since, according to IrvingLevin Associates, a research firm that tracks health-care transactions.”
The Obama administration did nothing about it because the distortion in pricing is going to lead to collapse of the private segment of our healthcare system. Once the private segment of the healthcare system collapses a progressive government hungry to have power and control over the populous will install a single party payer system.
As proven over and over again, a single party payer system does not work. The government has to outsource all of the infrastructure to administrative services. The government does not control the administrative services overhead. Also, the government does not want to develop another uncontrolled and inefficient bureaucracy like the VA Healthcare System.
A single party payer system will lead to increases in unsustainable deficits and decreasing healthcare services.
It will take many years for the public to recognize that a universal single party payer system is inefficient. The government will hide the system’s inefficiency from the public.
The government should make common sense rules, enforce those rules and get out of the healthcare administration business.
Medicare and Medicaid costs have not been recognized by the general public yet.
The VA inefficiency and lack of service by the VA Healthcare System has been recognized in the last two years by the general public. The government has assured the public that the VA Healthcare System is improving.
The insurance industry is trying to fight back.
“No hospital system should be able to exercise market power to demand contract agreements that prevent more competitively priced networks,” said Cigna’s chief medical officer, Alan Muney, in a written statement provided by the company.
The Trump administration is aware of all of these problems. President Trump is trying to figure out a way of negotiating a deal with all the providers who are taking advantage of consumers and the government. His administration’s actions have been delayed by the slow death of Obamacare.
If Obamacare was repealed last year I am sure the topic of hospital monopolies would be a hot topic of debate today.
President Trump is presently attacking the middlemen who have made drug prices so obscene. This is a big problem and an easier target.
“The effect of contracts between hospital systems and insurers can be difficult to see directly because negotiations are secret. The contract details, including pricing, typically aren’t disclosed even to insurers’ clients—the employers and consumers who ultimately bear the cost.”
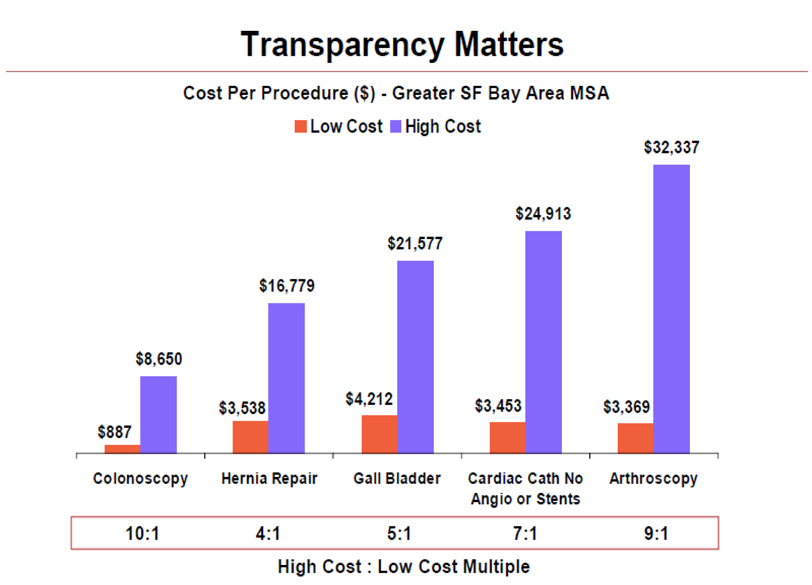
Hospital contracts forbids healthcare insurance companies to cover many procedures that can be performed as outpatient services outside the hospital environment. I have listed some of the price differences between the more expensive outpatient hospital care facilities and the independent ambulatory care facilities.
There are many examples of how hospital systems rip off consumers and increase the cost of healthcare insurance for all including employers, individuals and the government. It is also decreasing the access to care for all.
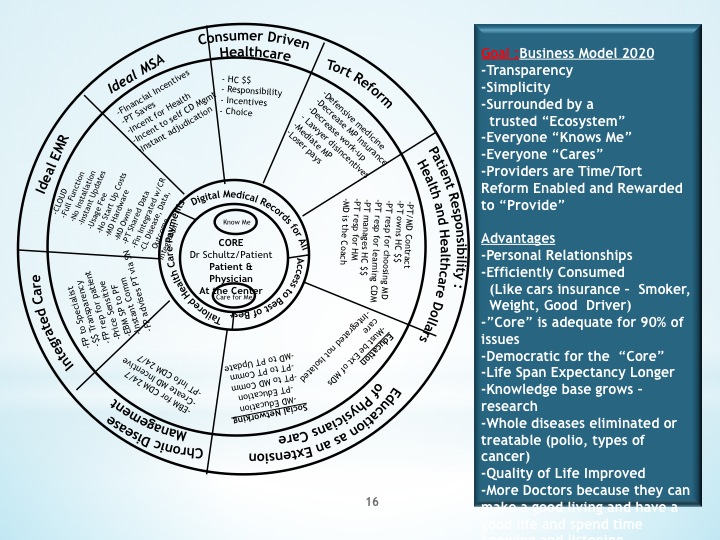
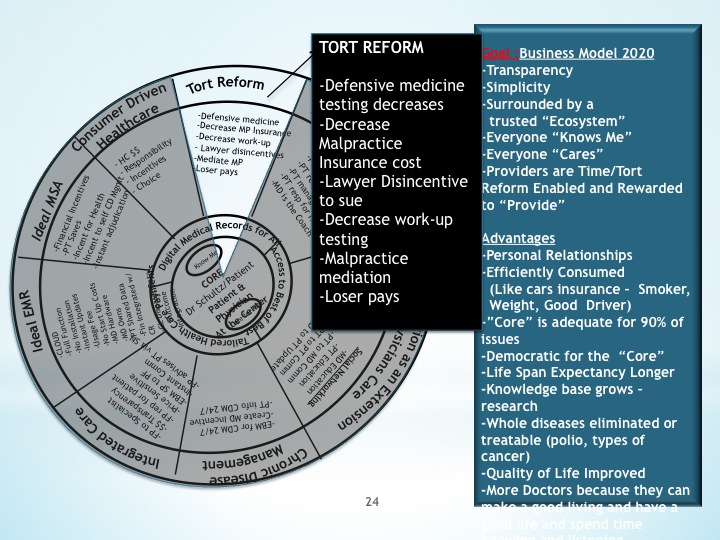
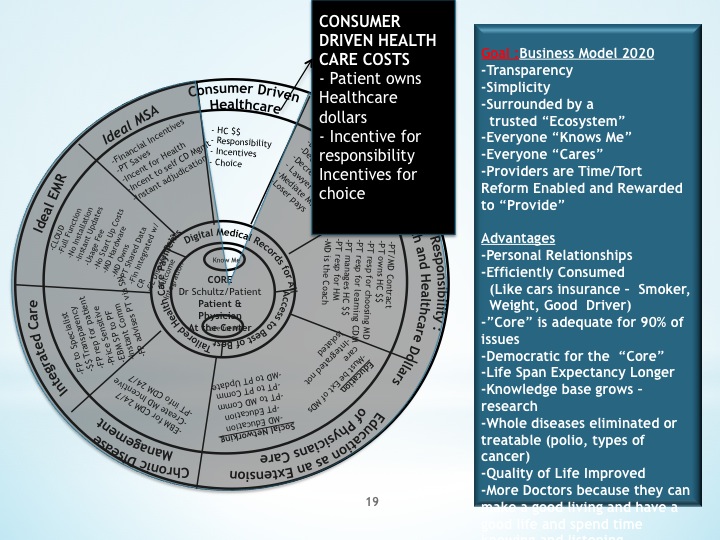
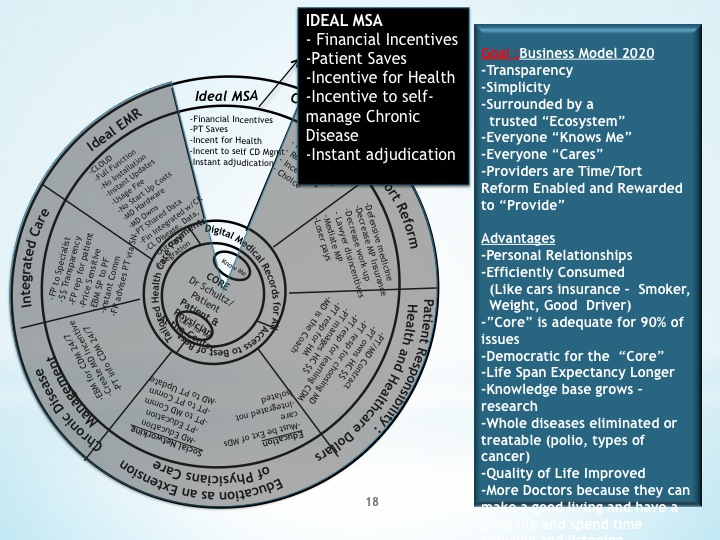
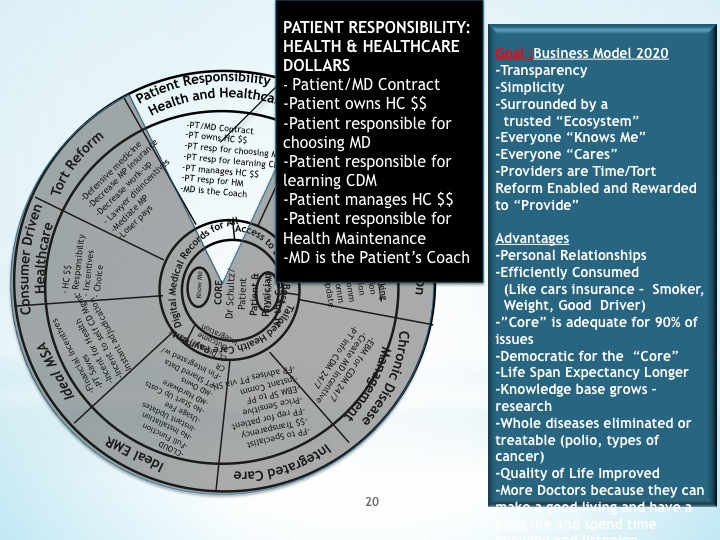
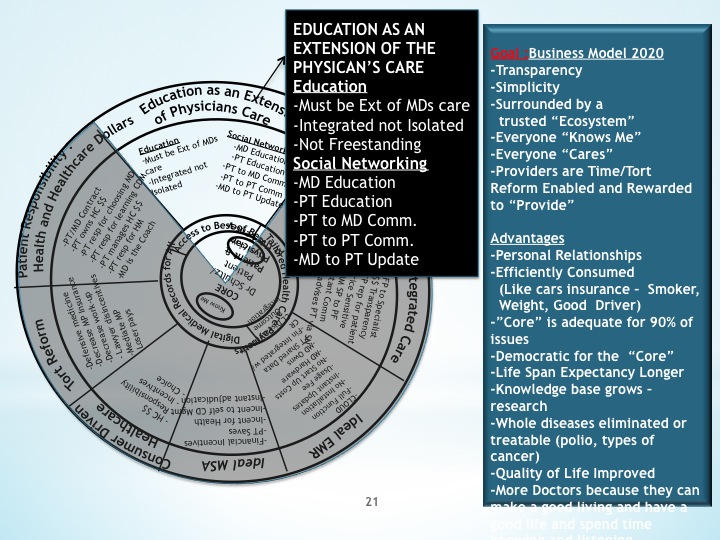
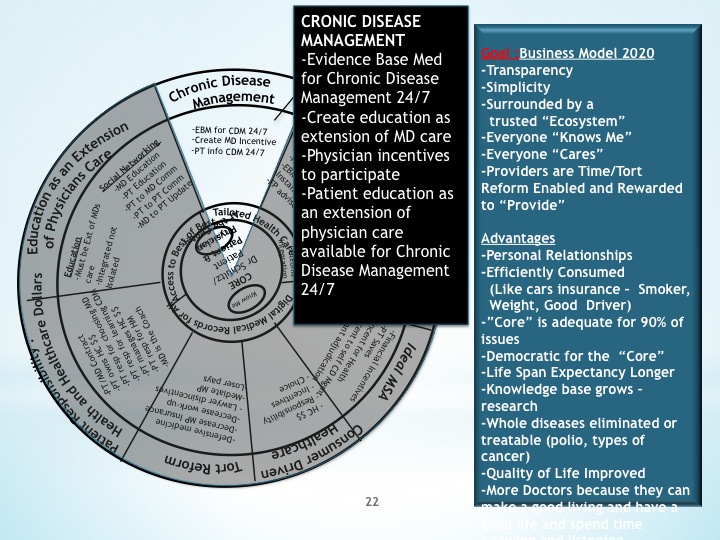
If the government is really looking for a system that would work it should look at my Ideal Medical Saving Accounts are Democratic.
The opinions expressed in the blog “Repairing The Healthcare System” are, mine and mine alone.
Copywrite 2006-2018
Please have a friend subscribe