The Anatomy of Healthcare Billing
Stanley
Feld M.D.,FACP,MACE
The start of exposing the real cause of healthcare inflation has begun. The billing and reimbursement system is
finally being questioned.
I hope the debate creates an uproar among consumers who are the most
important and most disadvantaged stakeholders in the debate. My hope is consumers will realize they
are pawns in the complex billing and reimbursement system created.
Consumers must also realize they have the power to demand control over their
healthcare dollars and not hope the government will protect them.
Steven
Brill’s article in TIME magazine started the debate. The demand for transparent
pricing has started. Steve Brill’s
numbers are far from accurate. However,the
pricing information is close enough to get consumers mad as hell.
The Centers for Medicare and Medicaid
Services finally released its massive database containing what 3,000 hospitals
charge for 100 of the most common medical procedures.
The database compares the hospital
“chargemaster” to the prices Medicare actually paid.
The reimbursement to hospitals is based
on the hospital system’s estimates of the actual hospital costs plus hospital
administrative overhead. These estimates are an error. The calculation should be the actual costs
and not an estimate of the actual cost.
The database only covers 100 of the
most common illnesses.
I have written about hospital
administrators’ salaries being in excess of 1 million dollars a year with many
being up to 15 million dollars a year. These salaries are included in the
overhead covered by Medicare payment.
I have questioned the appropriateness
of these massive salaries. In Boston there seems to be a contest between hospital
systems for which CEO gets a bigger salary.
Another important question is how many
hospital administrators in a hospital system get an excessive salary for the
value they add to medical treatment.
Who is worth more, a physician or a
hospital administrator?
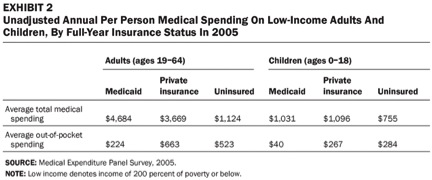
In many cases the
reimbursement by Medicare to some hospitals is 10% of the hospital’s billing. In other hospitals the difference is 20-40%.
The payment gap between hospital charges
for procedures and Medicare payments is also stunning. The average difference
between hospital charges for the 100 procedures tracked and what Medicare’s
average actually payment is a difference of 72%.
A good metric is to beware of the man
that quotes average percentages if you want to understand the actual
difference.
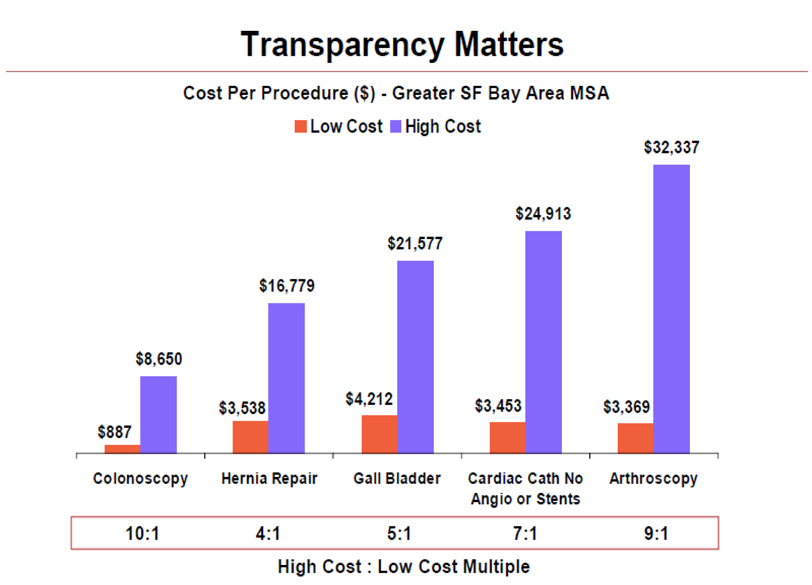
The best example I have seen to visualize the variation of these prices
in simple terms is as follows.
“That would be absurd. No
one would put up with it.
But it's how our health
care system works.”
Why should healthcare consumers in
America put up with it? Isn’t it the government’s job to protect us from this
abuse and not have a system that encourages it? Obamacare claims to stop the
abuse as it has been going on its merry way to encourage it.
This is not the entire grizzly story.
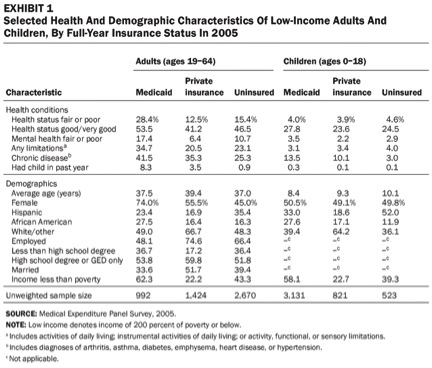
The average prices by states shows
massive discrepancies. In California, the average hospital charges $101,844 to
treat respiratory infections. In Maryland the average price for the same respiratory
infection is $18,144. The difference is 82% for the same disease in two
different states. The government is the same payer for both states.
New Jersey hospitals bill an average for
$72,084 for "simple pneumonia," while Massachusetts’ hospitals charges
an average of $20,722. Neither of the state’s hospitals receives that much
reimbursement for treating these infections from Medicare. However, New Jersey
hospitals receive more.
Uninsured patients and the indigent
without insurance are getting the shaft. These people will have to pay retail
hospital prices or get sued by the hospital system.
None of the hospital prices are
transparent. A patient cannot even beg the hospital system to get a price.
Many treatments can be administered as
an outpatient. The government pays at least three times more for chemotherapy
in a hospital setting or a hospital outpatient clinic as it would to a freestanding
private outpatient oncology clinic.
What’s the deal? The government doesn’t
trust physicians. It is afraid physicians will overcharge.
What does the government think the
hospital systems are doing?
I have also written about primary care
physicians’ salary being about $100,000- $120,000 a year. Surveys of physician
salaries have shown salaries varying between $100,000 to $600,000 per year. Surgical
subspecialists receive more than primary care physicians.
Let us assume the average physician’s salary
is $300,000 per year. There are approximately 600,000 practicing physicians in
the U.S.
The total physician reimbursement is $180
billion dollars a year in a $2.7 trillion dollar industry. This is less than
10% of the total dollars spent. Even if you doubled physicians’ salaries to
include an overhead of 50% physicians receive 13.2% of the healthcare dollars
spent.
A major question is where is the
remaining 2.5 trillion dollars going?
The healthcare insurance companies take
40% off the top of all care delivered including Medicare and Medicaid and other
government programs. They do all the government administrative services and
hide the fees through deductions that should go to expenses but with the
government’s permission go to direct patient care.
The most important metrics are never
discussed and inaccurately measured.
They are clinical outcomes and quality of procedures performed with
respect to financial outcomes.
The reason this measurement is not done
is because there is no accurate definition or measurement of these metrics.
Clinical outcomes as it relates to cost of care has to be included in the
measurement of quality of care. No one
knows how to do this.
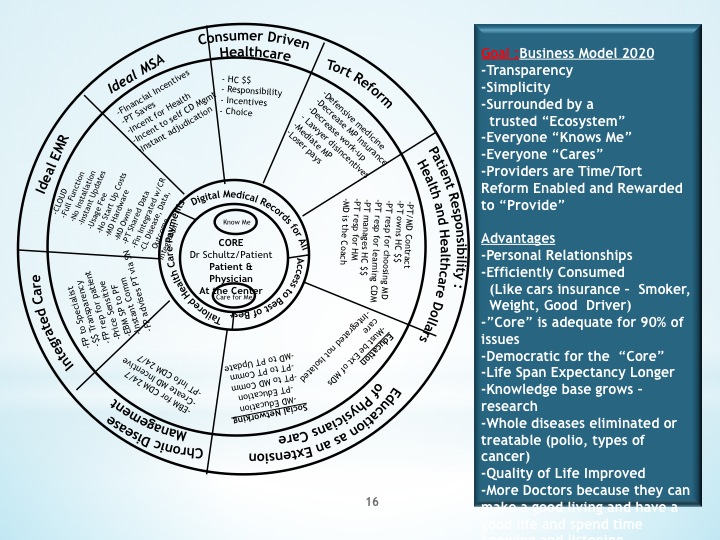
How does all this get fixed?
Consumers must drive the healthcare
system. My ideal medical saving account would go a long way in
dis-intermediating the healthcare insurance industry.
An easy to use web site should be constructed
using the Travelocity, Expedia or the Orbitz formula.
All hospital and physicians’ prices
should be online. All insurance and government reimbursement should be
published on this web site, plus
insurance premiums and their justifications. The real government overhead
should also be available to consumers.
A government web based educational
program to make consumers smart medical consumers would decrease healthcare
costs immediately.
All of the above would be a good start.
The opinions expressed in the blog “Repairing The Healthcare System” are, mine and mine alone
Please have a friend subscribe
Pretty section of content. I just stumbled upon your weblog and in accession capital to assert that I acquire in fact enjoyed account your blog posts. Anyway I will be subscribing to your feeds and even I achievement you access consistently fast.Everything For Sale http://www.shopforall.net