Stanley Feld M.D.,FACP,MACE
The only way America’s healthcare system will be repaired is by
revitalizing the Physician/ Patient Relationship.
Veterans complaining about the VA Hospital System in my last
blog brought on a flurry of negative comments about practicing physicians not
connecting with their Medicare and
commercial insurance patients in the private sector.
The chief complaint is that physicians are not connecting to
their patients or their patients’ illness. I have heard enough stories to
believe it is true.
A 44-year-old male with
private healthcare insurance sent one such complaint to me.
His acute illnesses history was compatible with acute prostatitis.
He needed a new physician because his previous primary care physician
had taken a sabbatical leave.
He called for help in finding a physician to his friends on
Facebook, Twitter and Link In. The consensus was the physician he describes
below.
The physician did multiple tests, several of which I did not
think were necessary, along with a cursory physical examination. The physician
thought the patient had prostatitis and prescribed Cipro for one month. A
follow-up examination was not scheduled.
The last paragraph in the patient’s note to me was,.
By the way, my doctor's office called to let me know the
lab results are in and they are mailing them to me. The doctor told the front
desk person to send me a letter, which I'll get in a day or two. According to
the front desk person, in the letter he says that my labs look good, and that I
need to work on getting my lipids up. Apparently he included a link to a
website that I can learn more about lipids. Pretty great patient care, eh…
This is horrifying to me. The patient will probably do well.
However there is no contact or concern about the patient’s outcome in this
interaction. There was no physician patient relationship formed for a patient
who is looking for a primary care physician.
I would be very upset if this interaction happened to me. I would be more upset if I then receive a bill
for $800 for the visit.
This patient does not know what the bill will be because the
office said it will bill his insurance company.
The evidence of the loss of the Patient-Physician Relationship of delivering medical care did not happen overnight.
A reader Dr. Dale Fuller sent me this commentary. He walks us through the
evolution of the destruction of the Doctor- Patient relationship.
Dr. Fuller’s view is similar to the view I have discussed in this
blog on multiple occasions. I believe it is important to publish his thought in
its entirety.
"Whatever Happened to
the “Doctor- Patient Relationship?”
Dale Fuller M.D.
Lately, I
find myself thinking about this question more and more. I think the first time I heard the term,
“doctor-patient relationship” was back during Harry Truman’s administration,
when there was an effort led by the Democrats to create a National Health
Insurance Program.
“Socialized
Medicine” the opposition cried, and “The end of the doctor patient
relationship! I wasn‘t even a student
in college back then, and in the absence of more information, I saw the
doctor-patient relationship in the context of my experience with the doctor who
looked after me on those rare occasions when I needed to see him,
Dr. T.D.
Jones, who was a very kind man. He was a
small town doctor, and the only doctor in my hometown as well as a good many
other towns around it during World War II.
I kind of
understood the term “socialized medicine” in the context of the then-new
National Health Service being launched in Great Britain.
Truman and
company lost the battle for NHI back then.
The next big
“Socialized Medicine initiative arrived in 1960
“Socialized during the Republican administration of Dwight
Eisenhower.
Senator
Robert Kerr, of Oklahoma and Rep. Wilbur Mills of Arkansas, both Democrats
introduced the Kerr-Mills act, the “Medical Assistance for Aged Act 1960-1965”
(benefiting primarily the elderly on Old Age and Survivors’ Assistance).
Kerr-Mills
was passed in 1960, again over cries that it would destroy the doctor-patient
relationship. But this time the cries
were neither so loud, nor as successful.
By this time I am a newly minted MD, and my awareness of the total
meaning of the term is still mostly intuitive.
During the
administration of Lyndon Johnson, came the Social Security Amendments of 1965,
which brought us Medicare and Medicaid.
When I
entered practice in 1968, Medicare and Medicaid were just getting under way, so
I never experienced what it was like to practice in the absence of the law.
In March of
2010, President Obama signed into law The Patient Protection and Affordable
Care Act, and we are now living through the incremental steps preceding that
law becoming fully in effect in 2014.
The various
legislative initiatives have, to be sure, impacted the doctor-patient
relationship in many ways, as the opponents predicted, but it appears to me
that we have been hearing less and less about that relationship as the years
have passed.
I think it
might just be that the relationship we are discussing may be threatened by a
number of other forces other than the laws described above, but before I
attempt to list those forces, I want to spend a little time setting the stage
to describe just what the doctor-patient might and might not mean.
Goold and
Lipkin, in an article published in 1999 (1) called the doctor-patient
relationship “a keystone of care: the medium in which data are gathered,
diagnoses and plans are made compliance is accomplished, and healing, patient
activation, and support are provided.”
They say that
the medical interview is the major medium of health care, and that more than
82% of diagnoses are made by history alone.
The three
functions of a medical interview are the gathering of information (both through
history and physical examination) developing and maintaining a therapeutic
relationship, and communicating information.
In the eyes
of the law, physicians also have a fiduciary responsibility toward their
patients. Physicians are bound to act in their patients’ interests even when
those interests may conflict with their own.
In that
physicians are often directly involved with events and conditions that are
life-altering for their patients and families, at birth, during severe illness,
healing or death, it can also be said that in being a physician, and providing
health care, doctors are engaging in a moral enterprise.
There was a
time when the unwritten social contract laid out above, simply existed as an
understanding between patients and doctors.
In the early
1940’s the arrival on the scene of what became the Blue Cross and Blue Shield
program, initially serving the employees of the Dallas, Texas Independent
School District began to interpose a third party, the insurance company,
working through the employers, in the social contract that was the Doctor-Patient relationship.
Initially
that interposition was pretty innocuous, with the insurance plan simply paying
the bills of the doctor as they were presented. The phrase, “usual and
customary” arose to define the fees involved that the insurance company paid.
Unusual fees or fees exceeding customary levels became subject to challenge,
requiring justification if they were to be paid.
Over time, a
database of fees that really were usual and customary began to become a better
and better tool to define where the usual kind of fee stopped and the unusual
kind of fee was recognized.
Kerr-Mills,
when it came along, introduced the federal government as a payer, and
relatively soon thereafter, the health care bureaucracy began to grow and
insert itself between doctors and patients to an increasing degree.
Since this
was in the “Pre-Medicare era” the number of patients involved was relatively
small, and so the impact on the doctor patient relationship was still somewhat
limited.
The arrival of Medicare and Medicaid served to
illustrate that the old “camel entering the tent” analogy was beginning to come
true.
Initially,
while the organizations were formed to administer the programs, “usual and
customary” was still the order of the day where payments were concerned, and
the social contract still functioned much as it had always done.
At the
request of the Department of Defense, organized medicine (AMA) created a set of
relative value scales in an attempt to standardize professional fees. The set
of codes was called “Current Procedural Terminology (CPT codes)” (first
introduced in 1966).
The charges
were to be based upon a blend of time required, professional skill involved,
and liability risk.
The compendium
of procedures have grown over the years, the principles remain essentially the
same.
In a fit of
zeal, the Federal Trade Commission inserted itself and accused professional
societies of “price fixing” via the CPT codes.
Settlements
eventually ensued, and money passed from the societies that were sued to the
FTC, and life, after the “nolo contendere pleas’ went on as usual.
The reason
for this was that the societies were not well enough funded to defend their
position vs. the FTC, even though they might have won their cases.
Increasingly
though, as might be expected, the government began to insert itself more and
more into the transaction between doctors and patients, generally, drawing upon
the reality that it was paying, directly or indirectly, for more than 50% of
the care given in the US.
Regulations
and rules have proliferated, respecting what can and cannot be done for
patients who are beneficiaries of federal programs.
Another force
was also becoming more vocal in making statements and policy regarding what
could and could not be done for patients.
This force
began with the passage of the Health Maintenance Act of 1973. This act enabled a vast acceleration of the
whole concept of managed care.
Healthcare
Insurance Companies citing the growing demand for, and cost of medical care to
employers, found a ready market among employers for their “products” to serve
as “benefits” for their employees.
Physicians
and hospitals, fearing that they might be left out of the managed care programs,
made haste to “join” this program or that program, seeking access to the
populations of patients enrolled in the programs by the insurance companies
selling coverage to employers.
The fear was
that exclusive arrangement with insurance companies would eliminate whole
populations of patients from providers who had not “signed up”.
This meant
that the traditional bilateral social contract between doctors and patients
essentially had come to an end of sorts.
Patients’ expectations
were that service and behavior of the doctor they were allowed to see remained
pretty much the same except for a small by important fact.
Those
employees covered by managed care were required to see the doctors who
participated in the program, and to use the hospitals the programs had
agreements with.
Financial
penalties awaited those patients who sought their care “out of plan”, for
whatever reason.
Now patients
and doctors both have someone else “calling the tune” when it comes to the
delivery of healthcare.
Each time the
“plan” purchased by the employer changed, for whatever reason, there could be a
change in the physicians and hospitals available to the patient.
This brings
us to a key element of the doctor-patient relationship. A key element is
continuity of care.
Continuity of
care brings with it an opportunity develop relationships in which doctors and
patients really know and trust one another. This relationship allows physicians
to recognize changes in patients and recognize the early onset of disease.
Neither the physicians’ understanding nor the
patients’ trust cannot be rebuilt immediately between two individuals each year
who are basically strangers to one another.
Doctor of days past, the trusted counselor, often
friend and confidant, is no longer exists.
Now, patients are simply seeing another person in an office. Both
parties are at sea when it comes to knowing what they need to know about one
another to allow the encounter to produce the necessary result within the time
allowed.
Time, like
continuity, is also a vanishing element in the doctor-patient
relationship. Fewer and fewer
practitioners have the time, amidst the pressures of “patient throughput” to
really engage in patients’ needs.
Physicians
must gather and record data, establish a diagnosis, and create a treatment plan
of quality.
The
documentation has to be complete in order to get paid by the government or the
healthcare insurance carrier.
Doctors must also
explain his treatment plan in such a way that they are assured of patients’
compliance with the treatment proposed in the time available to doctors.
As a result
of decreasing reimbursement and increasing overhead the time necessary for
patient education is insufficient. Patients do not understand the significance
of the therapy. The result is a lack of compliance.
Another
problem is that the “third party payers” rather than the patients approves of any
tests and procedures that doctors believe are needed to strengthen the
diagnosis.
The result is
a further erosion of patients trust in the doctor.
The time for
a consultation is short. Tests and procedures are now increasingly used to
substitute for the gathering of data to make the diagnosis.
Tests and
procedure escalate the costs of medical care.
Data
gathering by history and physical examination is time consuming. If a history
and physical examination is properly done it can yield the diagnosis of patients’
problems about 80% of the time.
The
doctor-patient relationship is indeed fading into the past. The third party carriers
and the federal government have, in their zeal to contain cost, pretty much
seen to that.
The reality
is that the destruction of the doctor-patient relationship costs more in the
long run.
The federal government, in its enthusiasm to
make a positive impact on the quality of care patients receive, has mandated
the use of electronic medical records.
The EMR in
its own way have also served to diminish the doctor-patient relationship.
In many
doctors’ offices, the focal point in the room is a computer with data entry.
The keyboard and the screen have almost the full attention of the doctor, who,
without looking at the patient, asks the questions and types the responses.
The patient is lucky if the doctor makes eye
contact with him/her for a brief interval a couple of times during the visit,
thus further diminishing the possibility that trust can be built in the
encounter.
The quality
of the encounter can, in the opinion of various policy makers and consultants,
be measured and changed in the same way that manufacturing processes can be
impacted by applying the principles taught by Deming and others.
Maybe it can,
but it has yet to be demonstrated.
Processes peripheral to the interaction of patient and doctor, may be
made better, but there is little evidence that the same approach can bring back
anything like the doctor patient relationship we used to know."
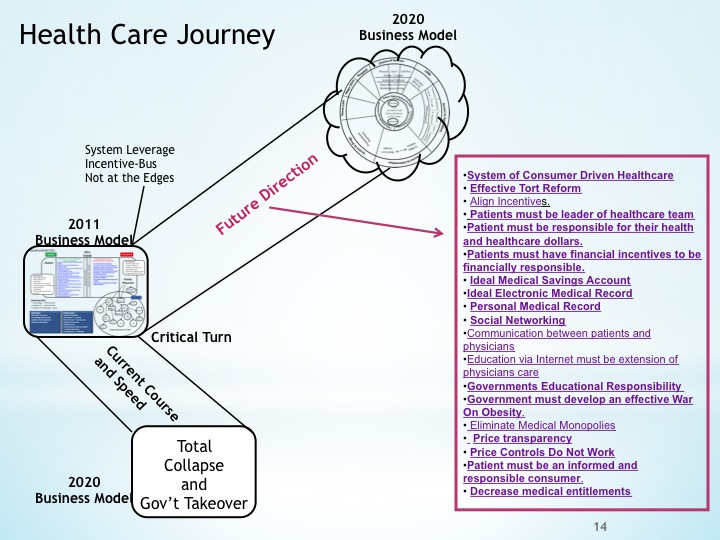
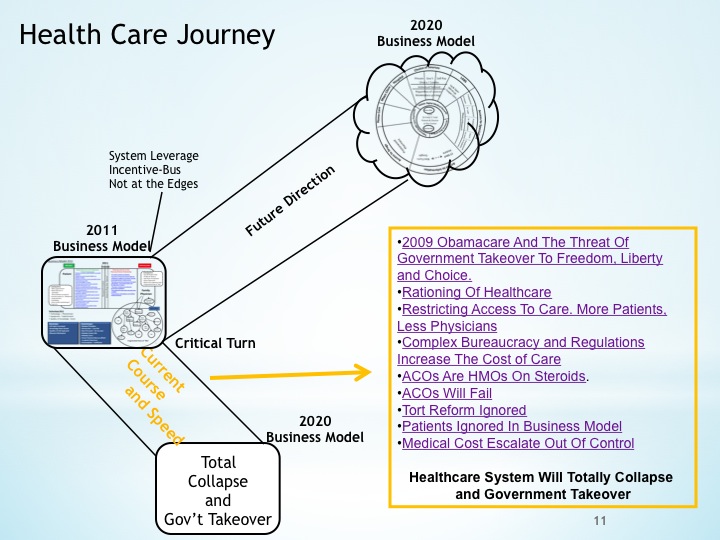
The three basic goals of Obamacare are
to create an affordable healthcare system with access to care of high quality.
A complicated and complex
bureaucracy that is over regulation will be very difficult to enforce.
It will penalize physicians’
judgment as it tries to decrease reimbursement. It will restrict patients’
access to medical care. It will reduce freedom choice.
Obamacare will not enhance the
Patient Physician Relationships that are so vital to a successful therapeutic
effect.
A healthcare system that places
consumers in control of their healthcare dollars and provides incentives to
consumers to be responsible for their health and healthcare will encourage
physicians to save money and rejuvenate the Physician Patient Relationship for
improved therapeutic outcome at an affordable cost.
The opinions expressed in the blog “Repairing The Healthcare System” are, mine and mine alone
Please have a friend subscribe
Very nice post. I just stumbled upon your blog and wanted to say that I have truly enjoyed surfing arond your blog posts. After aall I’ll be subscribing to your rss feed and I hope you write again soon!