A Bogus Attack For A Political End
Stanley Feld M.D., FACP, MACE
The New York Times continues to be a mouthpiece for the Obama administration. I suspect the editorial board thinks the only thing that will save the healthcare system in America is a government controlled single payer system.
This is President Obama’s goal even if he has to destroy the medical care system.
On September 20th, 2014 the front page top right hand column article in the Sunday New York Times was After Surgery, Surprise $117,000 Medical Bill From Doctor He Didn’t Know appeared.
In the past the New York Times reserved this spot for the most important story of the day.
This story was the most important news story on Sunday September 200h 2014. The Times thought it was more important than a story about the economy, ISIS, the mid-term elections, Israel, Hamas or Iran’s nuclear ambitions.
The story intended to inflame the New York Times’ readers so they would be angry at the medical profession.
The problem is that the story is peppered with misinformation and disinformation.
The New York Times writer used a typical Saul Alinsky tactic. Her goal was to prevent the opponents of the story from responding intelligently.
Public opinion will be on her side because the New York Times is supposed to be a credible source.
Saul Alinsky’s rules instruct one to lie if necessary. The next step is to frighten consumers into thinking the system under attack cannot work.
“Before his three-hour neck surgery for herniated disks in December, Peter Drier, 37, signed a pile of consent forms.”
Peter Drier did not read or modify the consent forms. He should have made the hospital and his doctor liable for any unauthorized expenses, providers, or events.
Peter Drier is a bank technology manager. Banks have their own small fine print intended to keep consumers liable and uniformed.
Peter Drier should have modified the consent forms before he signed them. He can refuse to authorize treatment or payment to any provider or procedure performed in the hospital that was outside of his insurance network.
In Network providers have to agree to accept the negotiated fee. If they need an additional provider it must be a provider that will accept the negotiated fee of his insurance company.
A bank technology manager who had researched his insurance coverage, Mr. Drier was prepared when the bills started arriving: $56,000 from Lenox Hill Hospital in Manhattan, $4,300 from the anesthesiologist and even $133,000 from his orthopedist, who he knew would accept a fraction of that fee.
Every consumer should find out if their providers are in their insurance network .
All of those prices are ridiculous retail prices. The real question is how much did his insurance company pay and how much is he liable for.
Peter Drier did not do a very good job in researching his insurance company’s coverage. A third party payer would never approve a $56,000 payment to the hospital for the proposed procedure.
Hospitals bill very high retail prices. They will negotiate a price that is 50-90
5 lower than the retail fee.
The author, ELISABETH ROSENTHAL, has a list of recent articles criticizing the healthcare system about exorbitant retail pricing.
- COLONOSCOPY: Colonoscopies Explain Why U.S. Leads the World in Health Expenditures
- PREGNANCY: American Way Of Birth, Costliest In The World
- JOINT REPLACEMENT: In Need Of A New Hip, But Priced Out of the US Market
- HOSPITAL PRICES SOAR: A Stitch Tops $5000
All of these articles criticize the retail price providers charge. They do not tell the reader what the providers receive as reimbursement by the government or the healthcare insurance company.
Consumers are the victims of the constant effort to try to reduce healthcare costs and stick consumers with the bill.
Obamacare has driven the healthcare insurance industry to raise premiums and decrease coverage in order to cover their supposed actuarial risk.
The decreased reimbursement by the healthcare insurance industry has driven providers to increase their fees for service. The hope is to occasionally catch a consumer who is uninsured and liable for the fee.
The uninsured consumer cannot afford the fee and therefore will not pay the fee. The provider then has to sue the consumer to collect whatever they can. The cost of the suit is not profitable for the provider. He usually writes off a loss.
President Obama and the government control advocates will use the resulting chaos in the marketplace to prove that a free market for healthcare system does not work. Therefore the country needs a government controlled single party payer system.
The problem with these horror articles is they frighten consumers. They do not address the reason that the healthcare industry costs $2.7 trillion dollars a year.
The chaos in the marketplace is the result of the government (Obamacare) involvement into the free market system.
I am also not sure if the $2.7 trillion dollars is from retail charges or negotiated payments. The answer to the question is totally opaque.
The reasons for the increasing costs are many.
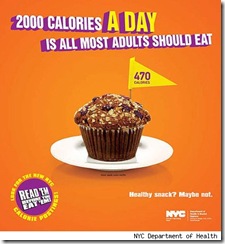
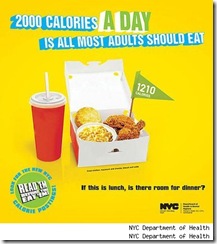
Americans are becoming less healthy because they are not being responsible for their health. It is hard to maintain weight when almost every restaurants main dish is higher than their daily caloric allotment.
The result is an obesity epidemic. Over 50% of Americans are Obese.
Obese individuals have a 40% increased incidence of chronic disease.
Controlling a chronic diseases can decrease the complication rate of those diseases by at least 50%.
If we ran the numbers we could reduce the healthcare costs below one trillion dollars a year.
Everyone complains about the grotesque profits the healthcare insurance companies make. Everyone understands the profits result from the inflated bureaucracies and double payments made to segments of the bureaucracy.
If one insurance company wanted to be competitive it would lower its premiums and overhead. All the other insurance companies would do the same to stay competitive.
One has only to look at the cell phone industry. Not only has the cost of the cell phones been lowered but monthly charges are continually decreasing.
One should also look at what ITunes did to the music industry.
The government should stop feeding the public disinformation leading to confusion of the facts..
President Obama's goal is to destroy the medical system so that consumers will believe the only thing that will work is a government controlled single party system.
Single payer systems throughout the world have proven to be unsustainable.
The healthcare system is dysfunctional. Medical care has been distorted at the consumers’ expense and for the profit of the profit of the healthcare industry.
America has to become innovative and build a healthcare system to the advantage of the consumer.
The solution
Is about consumers becoming aware.
Is about leadership.
Is about innovation.
Is about consumers being responsible for their health and their healthcare dollars.
The opinions expressed in the blog “Repairing The Healthcare System” are, mine and mine alone.
Please have a friend subscribe
I think the admin of this site is in fact working hard for his web page, as here every material is quality based information.